The study, based on data from The Danish Chiropractic Low Back Pain Cohort (ChiCo) and including 2,777 patients, examined differences across three age groups: under 40 years, 40–59 years, and 60 years or older. Patients were followed for up to one year.
Small differences across age groups
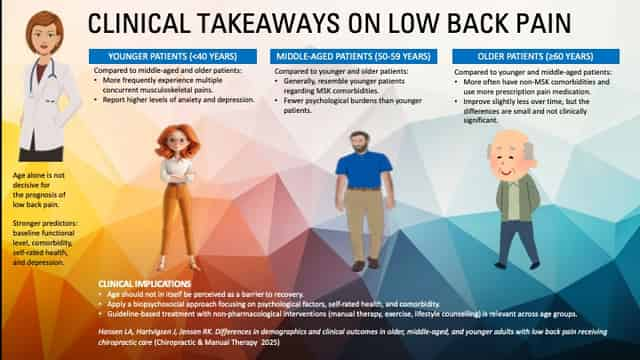
At baseline, the age groups had a similar functional level, measured with the Roland Morris Disability Questionnaire (RMDQ). However, older patients more often reported other illnesses and the use of prescription pain medication, while younger patients more frequently experienced depression, anxiety, and multiple concurrent musculoskeletal disorders.
Depression and anxiety were evaluated using two questions from the Danish version of the Örebro Musculoskeletal Pain Screening Questionnaire (OMPQ)1, based on the PICKUP model2. Depression was assessed by: “How much have you been bothered by feeling depressed in the past week?” and anxiety by: “How tense or anxious have you felt in the past week?”, both rated on a 10-point scale (0 = Not at all/Absolutely calm, 10 = Extremely/Very tense).
All age groups improved over time, but older patients consistently showed a slightly lower degree of improvement. The differences, however, were too small to be considered clinically significant.
The most important prognostic factors
The analysis pointed out that the most significant risk factors for prolonged functional problems were not age, but rather:
- high level of disability at baseline
- multiple musculoskeletal disorders
- poor self-rated health
- and high levels of depression and anxiety.
Clinical significance
The researchers conclude that age in itself is a weak predictor of the course of low back pain. For chiropractors and other healthcare providers, this means that elderly people can be helped when they see a chiropractor and that focus should be on the patient’s overall health profile and psychological well-being rather than age alone.
The study thus supports a biopsychosocial approach to treating low back pain, where a holistic, guideline-based effort is central – regardless of the patient’s age.
1Kent P, et al. The concurrent validity of brief screening questions for anxiety, depression, social isolation, catastrophization, and fear of movement in people with low back pain. Clin J Pain. 2014;30(6):479–89.
2Traeger AC, et al. Estimating the risk of chronic pain: development and validation of a prognostic model (PICKUP) for patients with acute low back pain. PLoS Med. 2016;13(5): e1002019.
Louise Aagaard Hansen, Jan Hartvigsen, Rikke Krüger Jensen. Differences in demographics and clinical outcomes in older, middle-aged, and younger adults with low back pain receiving chiropractic care. Chiropractic & Manual Therapies 2025.
Would you like to know more?

